Stereotactic radiosurgery alone is the preferred method for treatment of patients with cancer metastases to the brain according to the results of several clinical studies.1,2

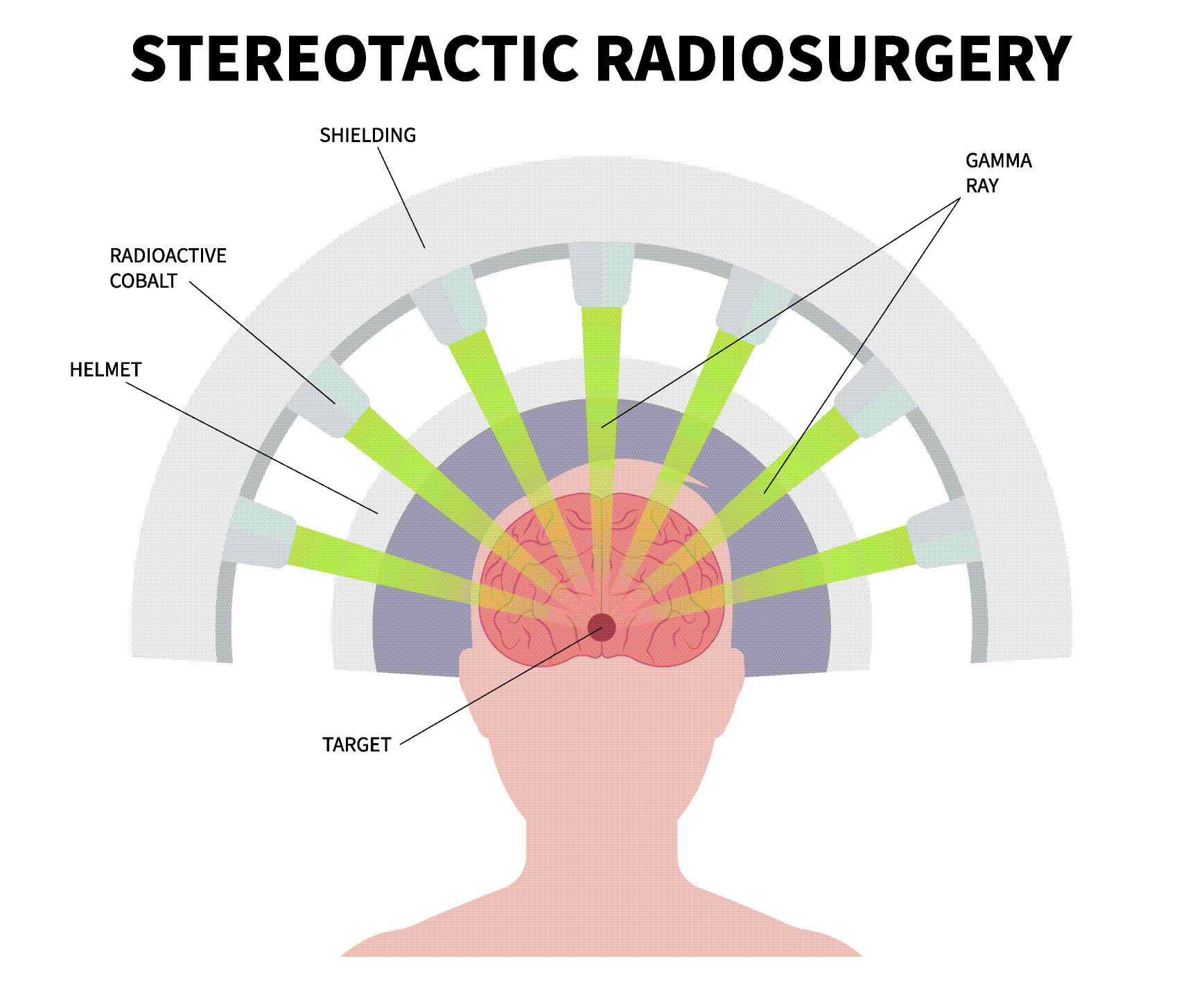
For decades, whole-brain radiation therapy (WBRT) has been the standard treatment for patients with brain metastases. However, stereotactic radiosurgery (SRS) is a more precise treatment that delivers a high dose of radiation to a highly defined target—in other words, the radiation is delivered directly to the cancer while sparing the healthy surrounding tissues. In recent years, SRS combined with WBRT has shown a survival benefit over WBRT alone. Now, however, researchers are evaluating whether SRS alone can provide the same benefit to patients while subjecting them to fewer side effects.
Researchers from the M. D. Anderson Cancer Center conducted a study that included 58 patients who had one to three brain metastases. The patients were assigned to receive SRS alone (30 patients) or SRS plus WBRT (28 patients). The study was stopped early due to a decline in learning and memory function four months post-treatment in patients receiving SRS plus WBRT—52% of patients receiving SRS plus WBRT were likely to have significant learning and memory decline compared with 24% of those receiving SRS alone.

Most recently a prospective, multi-center phase 2 study brings highlighted that patients with small cell lung cancer (SCLC) who have developed brain metastases also benefit fro the targeted stereotactic radiosurgery (SRS) approach which appeared equally effective and potentially less harmful.
Key findings from the study include:
- 100 patients with 1-10 brain metastases from SCLC were treated with SRS or stereotactic radiotherapy (SRT).
- The median overall survival was 10.3 months.
- Only 11% of patients experienced neurologic death at one year, which is lower than expected based on historical data from WBRT treatments.
This research is significant because it challenges the long-standing belief that WBRT is necessary for SCLC patients with brain metastases. SRS, which delivers high-dose radiation to specific areas of the brain, may offer a less invasive alternative with fewer side effects. The study’s results are encouraging for patients and oncologists alike, as they suggest that SRS could potentially replace WBRT in many cases, potentially leading to better quality of life for patients while still effectively managing their brain metastases.
Patients should consult with their healthcare providers to determine the best treatment approach for their individual cases. This study opens up new possibilities for personalized care in the challenging landscape of SCLC brain metastases – SRS alone (in addition to close monitoring) is the preferred treatment for this group of patients in order to preserve quality of life, learning, and memory.
Overview of Small Cell Lung Cancer
Join the Conversation on CancerConnect!
Reference:
- Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomized controlled trial. Lancet Oncology. 2009; 10: 1037-1044.
-
Aizer A, Bi WL, Catalano P, et al. Stereotactic radiosurgery in patients with small cell lung cancer and 1-10 brain metastases: A multi-institutional, phase II, prospective clinical trial. JCO. 2024;42:Abstract 2020.